Let’s be real for a second. There’s so much medical information out there, especially with AI being used in clinical decision-making. It’s actually kind of scary.
If you are a clinician, you know the feeling. You’re in the middle of a busy clinic day, maybe running twenty minutes behind, and a patient presents with a complex set of symptoms that rings a bell but you can’t quite pin down the latest guidelines for. You have about three minutes to make a decision.
In the past, you might have pulled a thick textbook off the shelf, but now you can access evidence-based resources at the point of care. Then, maybe you switched to frantically Googling, hoping to dodge the patient forums and land on a reputable study. Or perhaps you logged into UpToDate, which is fantastic, but sometimes feels like reading a novel when you just need a haiku.
Enter OpenEvidence!
You might have heard the buzz. Maybe a colleague mentioned, “I’ve been using OpenEvidence for the last week, and it’s incredible.” Or maybe you saw a headline about the first AI in history to score above 90% on the United States Medical Licensing Examination (USMLE).
But what exactly is it? Is it just another ChatGPT wrapper? And most importantly for us here in Canada, can we actually use it, and should we trust it?
I’ve spent some time digging into this medical information platform, and I think it’s something every health care professional needs to at least look at. It represents a shift in clinical decision-making—moving from keyword searching to actual intelligent synthesis of AI applications in healthcare. peer-reviewed medical literature.
What Is OpenEvidence? (Beyond Just “Medical ChatGPT”)
So, what is this thing?
At its core, OpenEvidence is the world’s leading AI-powered medical search engine designed specifically for clinicians. Note the distinction: it’s not a chatbot built to write poetry or code; it is a Tool for medical professionals to leverage AI applications in improving patient care. professionals to answer clinical questions using open evidence
OpenEvidence was founded with a very specific mission of helping physicians sift through the noise. The team behind it includes Daniel Ball and others who realized that the volume of medical data doubles every few months. No human brain can keep up with that.
The platform was developed with support from the evidence-based clinical community. Mayo Clinic Platform Accelerate program and has backing from heavy hitters like Google Ventures. This isn’t a garage project. It’s a serious medical information platform for health care that is trying to solve the problem of medical information overload and find the needle in the haystack.
Grounded in Reality, Not Hallucinations
We’ve all played with AI tools like OpenEvidence or ChatGPT. You ask ChatGPT a medical question, and it gives you a beautifully written, confident answer. But if you ask it for citations, it might make them up. It might reference a study by “Dr. Seuss” published in 1999 if you aren’t careful, but the AI platform helps filter for quality evidence. That’s called hallucination, and in medicine, it’s dangerous.
OpenEvidence is transforming This dynamic is influenced by the increasing use of medical AI in practice.
It is strictly grounded in the peer-reviewed medical literature, especially when used AI to filter the most relevant studies. When you type in a clinical question, it doesn’t just guess the next word in the sentence. It reads through millions of papers—from the New England Journal of Medicine, JAMA, The Lancet, and others—and synthesizes an answer based only on that evidence.
Then, it shows its receipts. Every claim has a little number next to it. You click the number, and it takes you to the abstract or the full text of the paper. It’s transparent.
Key Features for Canadian Clinicians
Why should a doctor in Toronto, Vancouver, or a rural community practice and medical director in Nova Scotia care about this?
Because time is our scarcest resource.
The “DeepConsult” Capability
The platform uses something they call “DeepConsult.” It’s designed to handle nuance. You don’t have to search “hypertension guidelines elderly.” You can type:
“85-year-old female with resistant hypertension, history of falls, and CKD stage 3, as noted by physicians at the point of care.” What is the evidence for spironolactone vs. eplerenone?”
OpenEvidence provides a synthesized answer that weighs the risks and benefits, citing recent trials. It acts like an AI agent that has read every paper on the topic in the last 24 hours.
Partnerships with the Giants
One thing that makes OpenEvidence the world’s leading medical information platform is its access. They aren’t just scraping the web for random information; they rely on curated evidence-based sources. OpenEvidence announced partnerships with content providers.
They have agreements with the leading evidence-based clinical organizations, including the American Medical Association, to enhance their clinical decision-making. Journal of the American Medical Association (JAMA) network, the American Academy of Family Physicians, and the American College of Emergency Physicians.
This means when you search, you aren’t getting blog posts. You are getting high-quality, clinically relevant evidence From the sources we already trust, we can explore the application of AI in medical decision-making, particularly in the context of the US medical licensing exam.
Powering the Workflow
There’s talk about using this technology to power all clinical workflows. Imagine an AI scribe powered by artificial intelligence that not only listens to the visit but automatically pulls up relevant guidelines for the condition you just diagnosed. That’s the future OpenEvidence is transforming healthcare towards.
They even have features like the ability to assess care professional status before using the AI tools. OpenEvidence dialer (in some regions) and optional visits integration, aiming to make the tool a seamless part of the day, not just another tab to open.
How to Access OpenEvidence in Canada
Here is the tricky part, and the part you need to pay attention to.
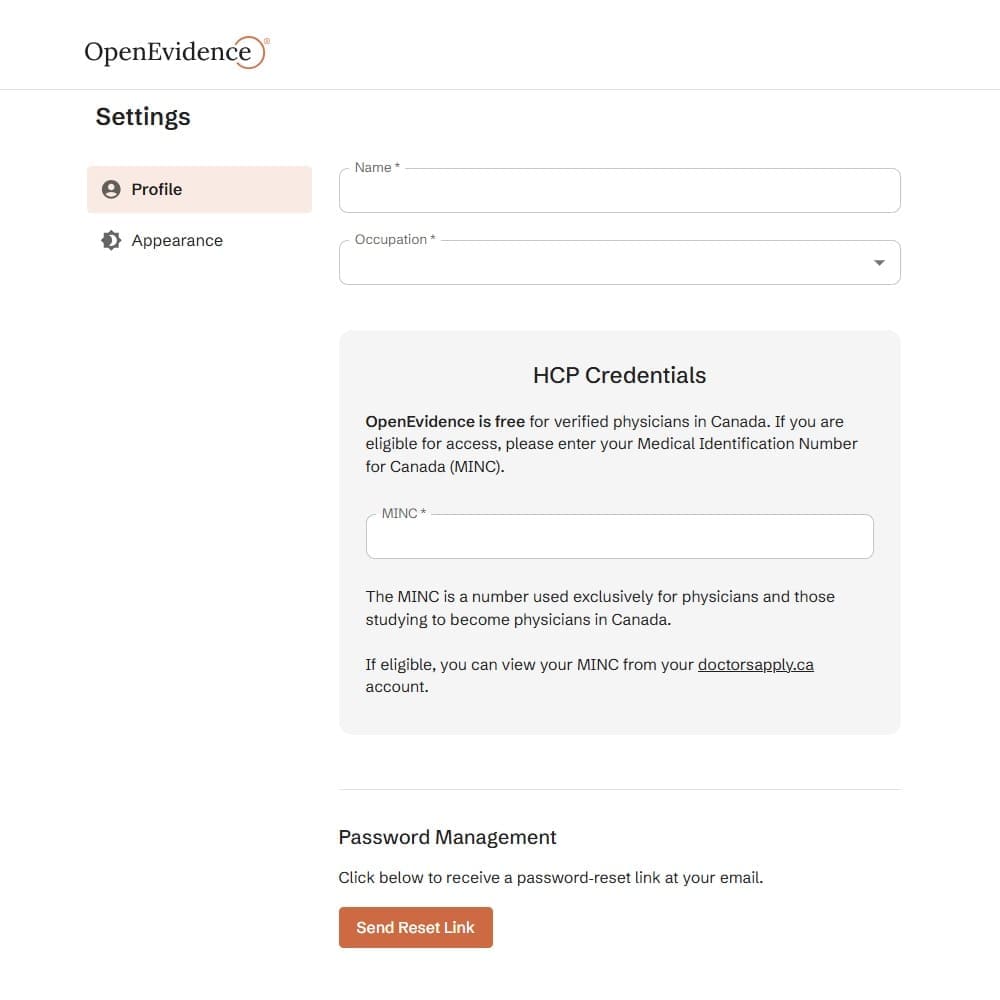
OpenEvidence is only available for health care professionals. You cannot just sign up with a Gmail account and start searching. This is a safety feature. They do not want patients using this for self-diagnosis because, powerful as it is, it requires clinical judgment to interpret.
The Verification Hurdle
Users, including medical directors of a community, can benefit greatly from these advancements. must verify their health care professional status.
In the US, they check the United States Medical Licensing number (NPI). For us in Canada, the system is slightly different but the principle is the same. You will need to prove you are a licensed professional.
You must verify their health care professional status usually by providing professional details that can be cross-referenced. Sometimes this involves a work email validation or uploading credentials. It ensures that the platform for health care professionals remains exactly that—a professional space.
If you are a student at Harvard Medical School or University of Toronto, you can often get access via your institutional email.
Is it Free?
As of right now, for verified clinicians, it is largely free to use the core search features. This is a massive advantage over verified subscriptions that can cost hundreds of dollars a year. They are betting on growth and potentially enterprise licensing (selling to a medical center or hospital system) to make money, rather than charging the individual physician.
Clinical Application: When to Use It?
So, when do I actually use this?
I’ve found it most useful for “grey zone” questions. The stuff where guidelines are vague or conflicting.
For example, I was seeing a patient recently with a weird presentation of gout. Standard therapy wasn’t working. I asked OpenEvidence: “Management of refractory gout in patient with sulfa allergy and CKD.”
In about ten seconds, it gave me a summary of three different management strategies, noting the renal dosing adjustments for febuxostat, and cited a recent review from the Mayo Clinic.
It’s also great for family medicine practitioners who have to know a little bit about everything. One minute you are a cardiologist, the next a dermatologist. AI is transforming how generalists maintain broad competency.
A Word of Caution
However, I treat it like a very smart medical student.
If a medical student told me, “Hey, I read this paper and it says we should give drug X,” I wouldn’t just write the script. I’d say, “Show me the paper.”
You have to do the same here. Verify their health care professional status? Yes. But also verify the answer. Click the link to access the platform OpenEvidence. Read the abstract. Ensure the AI didn’t misinterpret “associated with” as “caused by.”
Clinicians using OpenEvidence need to maintain that skepticism. It’s a tool to find evidence to help you decide, not a tool to decide for you.
Trust and Reliability: The “Evidence” in OpenEvidence
Can we trust it?
Well, OpenEvidence is the first AI to pass the medical licensing exam with such high flying colors. That proves it has “knowledge.” But knowledge isn’t wisdom.
The reliability comes from its constraints. Unlike ChatGPT, which is designed to be conversational and creative, OpenEvidence is designed to be factual. It is penalized (in its programming logic) for making things up.
It sources data from the American Medical Association, New England Journal of Medicine, and other titans. It’s essentially a super-fast librarian.
Dr. Antonio Jorge Forte from the Mayo Clinic has said things like OpenEvidence can power all clinical decision tools in the future. Dr. Ram Dandillaya from Cedars-Sinai Medical Center has also spoken to its utility. When you have validation from people at Cedars-Sinai Medical Center and Harvard Medical School, it adds a layer of comfort.
But remember, it is software. It doesn’t have a license to practice medicine. You do.
Comparison: OpenEvidence vs. UpToDate vs. ChatGPT
Let’s break it down simply.
- UpToDate: evidence-based clinical decision support This is the gold standard. It is written by human experts. It is trustworthy, but it is slow to update (relatively) and can be dense. It’s a textbook that discusses the use of AI in improving patient outcomes.
- ChatGPT: This is a genius improv artist. It knows a lot, but it lies confidently. It is not connected to a live medical library in the same rigorous way. It is risky for patient care.
- OpenEvidence: This is the hybrid. It has the speed and natural language understanding of ChatGPT, but it is shackled to the medical literature. It synthesizes advanced medical research instantly.
AI tools like OpenEvidence are filling the gap between the static textbook and the chaotic open internet.
FAQ
What is the use of OpenEvidence?
Why is OpenEvidence good?
What can OpenEvidence do?
Is OpenEvidence better than ChatGPT?
Is OpenEvidence a medical device?
Is OpenEvidence free for everyone?
Can I use OpenEvidence as a nurse?
Is OpenEvidence free for nurses?
Who can access OpenEvidence?
Who uses OpenEvidence?
Does OpenEvidence hallucinate?
How secure is OpenEvidence?
Can OpenEvidence make a presentation?
Can I upload documents to OpenEvidence?
Who is the CEO of OpenEvidence?
Who built OpenEvidence?
Who funds OpenEvidence?
Is OpenEvidence a public company?
Can I buy OpenEvidence stock?
Can I invest in OpenEvidence?
What is the DeepConsult feature?
Does OpenEvidence have a mobile app?
How does OpenEvidence make money?
Can medical students use OpenEvidence?
What sources does OpenEvidence use?
Is OpenEvidence HIPAA compliant?
How accurate is OpenEvidence?
Can OpenEvidence write clinical notes?
Does OpenEvidence offer a dialer?
Is OpenEvidence available in Canada?
How do I verify my account?
Can dentists use OpenEvidence?
What if OpenEvidence cannot find an answer?
Does OpenEvidence support image analysis?
How fast does OpenEvidence answer?
Can pharmacists use OpenEvidence?
Does OpenEvidence save chat history?
Is OpenEvidence owned by Google?
What is the valuation of OpenEvidence?
How does OpenEvidence help with burnout?
The Future of OpenEvidence in Canadian Healthcare
OpenEvidence continue its mission to organize the world’s medical knowledge. For us in Canada, dealing with long wait times and resource constraints, having an efficiency tool like this is a godsend.
AI is transforming healthcare, not by replacing doctors, but by removing the friction of finding information.
If you haven’t tried it, I’d encourage you to go to their site. Verify their health care professional status (it takes a few minutes), and just play with it. Ask it a question about a case that stumped you last week.
You might find yourself saying, “I’ve been using OpenEvidence for the last week, and I don’t know how I practiced without it.”
Just remember: It’s a tool. You are the doctor. Use it wisely.